
About the author
Dr. Roland Glauser (Zürich, Switzerland) earned his dental degree and doctorate from the University of Zürich, where he also specialized in prosthodontics, periodontics, and oral surgery. He held academic posts in Zürich and at Augusta University (USA), and has led several clinical and entrepreneurial ventures, including founding Cosmodent Clinic. With over 70 scientific publications and 14,000+ citations, he is an internationally recognized expert, serving as advisor, reviewer, and board member for leading dental organizations and companies.
Case information
Patient information: Male, 48 years old. Initial situation: Tooth gap in region #35. Soft-tissue thickness of 3 mm. Slight horizontal ridge collapse. Caries on adjacent crowned tooth #36. Surgical solution: Modified mini-roll flap was mobilized. Osteotomy was prepared according to protocol for D3 bone. Implant was inserted in region #35 at low speed and to a final torque of 11 Ncm. Restorative solution: Glass fiber post was cemented and prepared 3 months post-surgery. Full-arch impression was taken. Partially veneered and individually characterized zirconia single crowns for implant #35 and tooth #36 were cemented. Time of implant placement: Spring 2022. Follow-up period: 4.5 years.
The patient had tooth #35 extracted elsewhere (the diagnosis at the time was deep caries and acute pulpitis). Eight weeks later, he presented to my practice requesting a fixed restoration in this area. His medical history revealed controlled Type 2 diabetes mellitus, a smoking habit of 20 cigarettes per day, regular benzodiazepine use and poor oral hygiene (bleeding on probing index: 38%). For this patient, an implant system was required that
could integrate successfully under the challenging conditions of a high-risk patient and ensure long-term function and tissue health. A recent long-term study has demonstrated the ability of the Patent™ Implant to minimize the risk of inflammatory peri-implant conditions, such as peri-implantitis, in high-risk patients like the patient described (Karapataki 2023).
Initial situation

Lateral view 3 months after tooth extraction.

Radiograph 3 months after tooth extraction and before implant insertion.

Occlusal view 3 months after tooth extraction: slight horizontal ridge collapse.
Surgical procedure
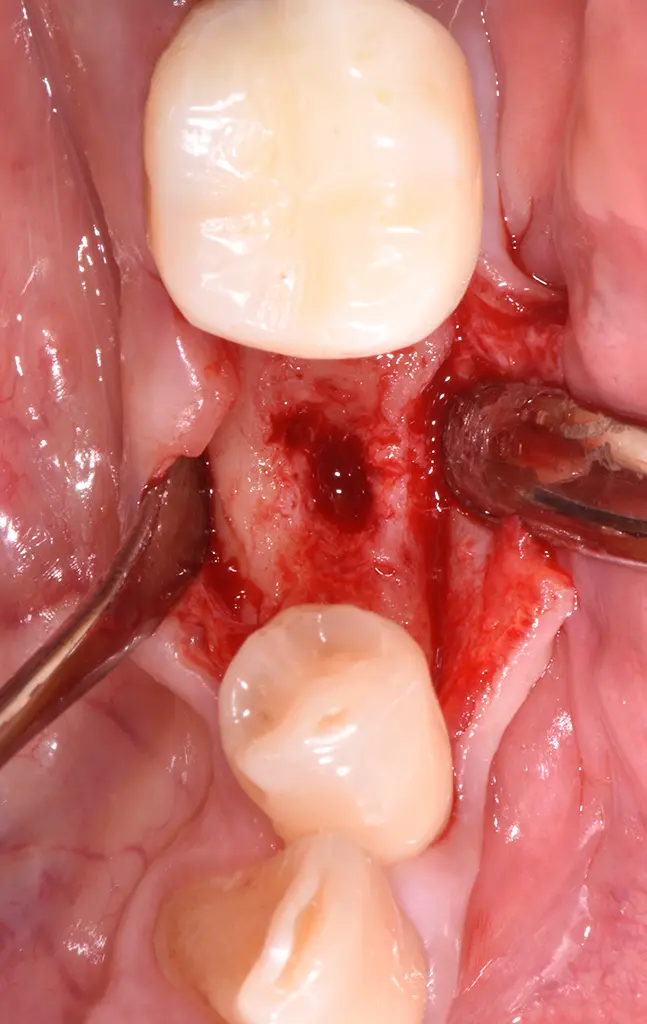
View of the bone crest after preparation of a modified mini-roll flap.
Prepared implant site after using the screw tap.
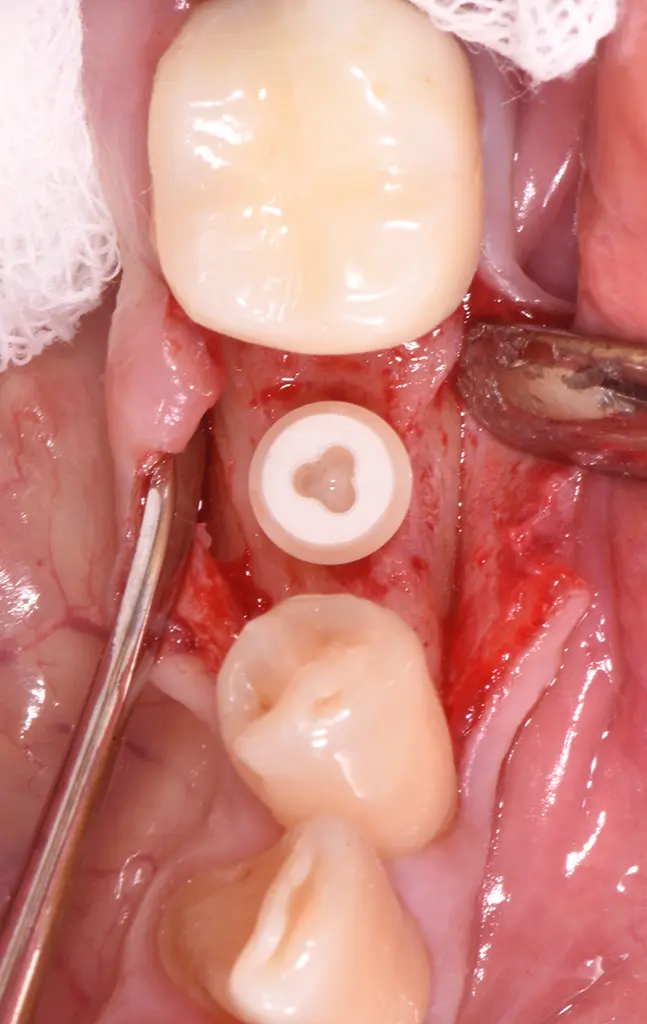
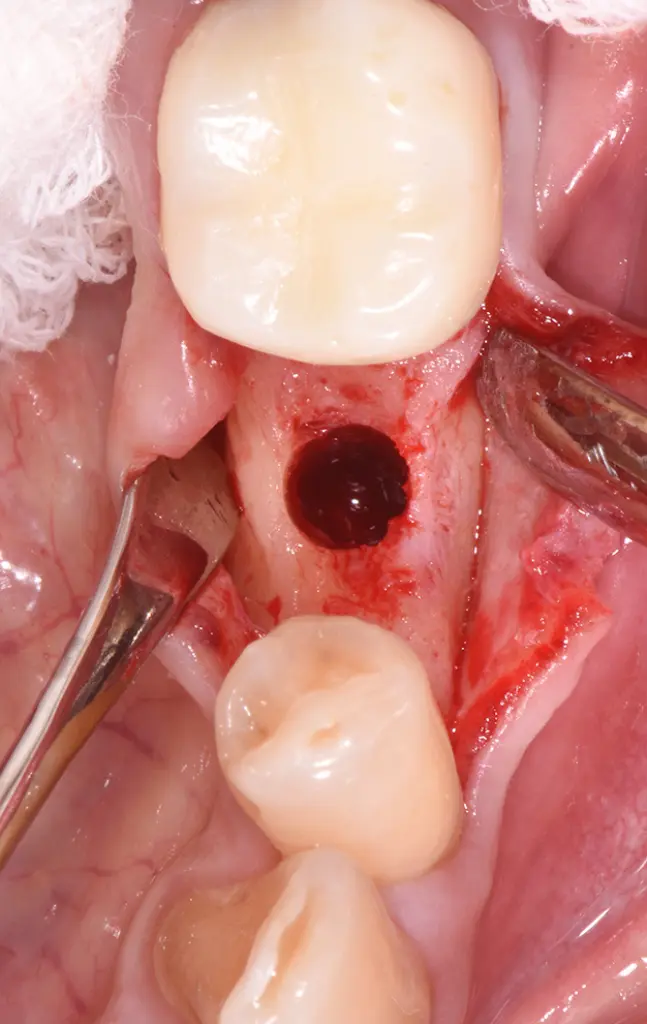
Two-piece Patent™ Implant horizontally optimally aligned.

Two-piece Patent™ Implant vertically correctly aligned.
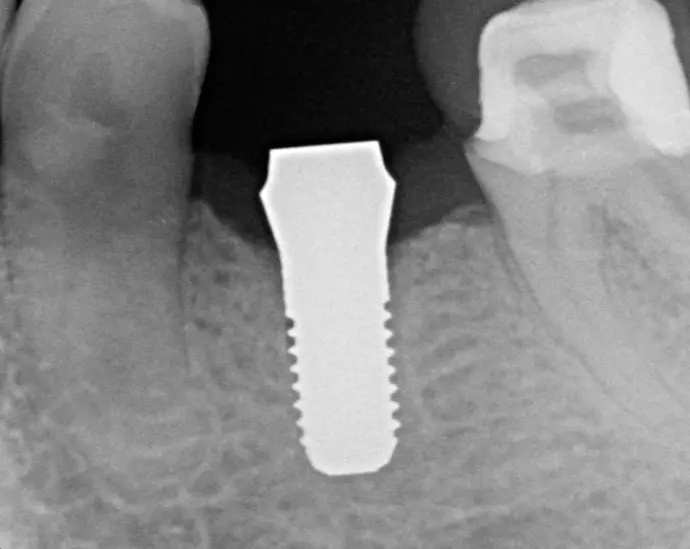
Post-op radiographic control.
Soft-tissue healing
Situation after suturing of the surgical site.

Situation 5 days post-op: stage-appropriate healing.

Situation 2 weeks post-op: nonirritated soft tissue.

Clinical situation 6 weeks post-op: nonirritated soft tissue.

Situation 12 weeks post-op: nonirritated soft tissue.
Restorative procedure

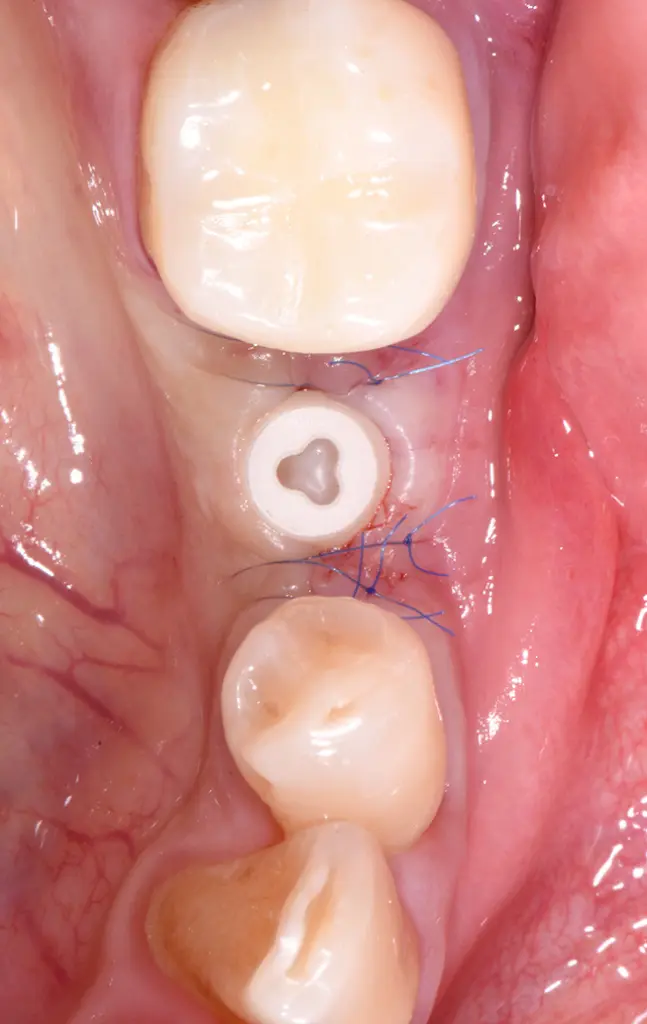
Prosthetic restoration 3 months post-surgery: Gingival retraction cord around implant #35.

Cemented glass fiber post.

Intraorally prepared glass fiber post.

Veneered, individually characterized zirconia crowns for implant #35 and tooth #36.

Situation after cementation of single crowns for implant #35 and tooth #36 in
subsequent session.
Follow-ups after 3 and 4.5 years

Situation 3 years post-op: healthy and stable soft tissue and excellent esthetics.
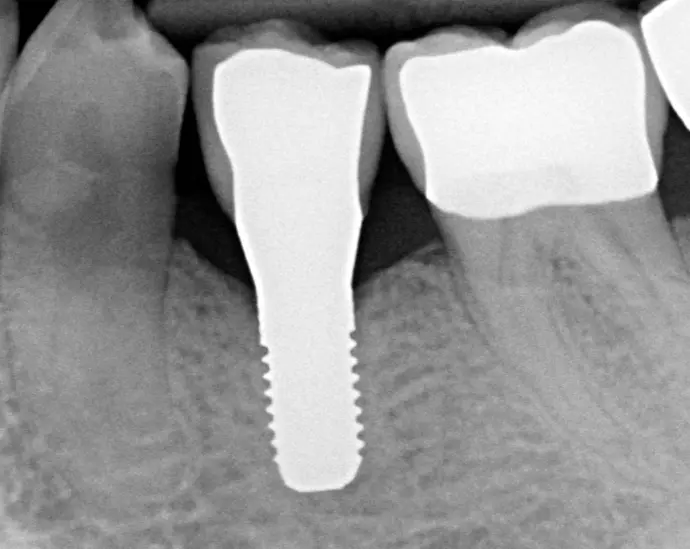
Radiographic control 3 years post-op: stable marginal bone level.

Situation 4.5 years post-op: healthy and stable soft tissue, shallow probing depth.





