CLINICAL CASES
DISCOVER OUR SELECTION OF
CLINICAL CASES

SINGLE TOOTH RESTORATION IN A PATIENT WITH RISK FACTORS
Tooth 35 was extracted. 8 weeks later, a symbionic tooth was placed. 4.5 years post-insertion, the site showed stable, healthy soft tissue and shallow probing depths.

SINGLE TOOTH RESTORATION WITH AN INDIVIDUALIZED SYMBIONIC TOOTH
A failing restoration (45–47) was removed, and a symbionic tooth was placed at site 46. All sites received single crowns. Six years post-op, site 46 showed healthy soft tissue.

IMMEDIATE PLACEMENT OF SYMBIONIC TEETH IN THE ESTHETIC ZONE
Failing restorations of teeth 11 and 21 were removed and the tooth roots extracted. Two symbionic teeth were immediately placed and later restored with single crowns.

SINGLE TOOTH RESTORATION IN A PATIENT WITH RISK FACTORS
Tooth 35 was extracted. 8 weeks later, a symbionic tooth was placed. 4.5 years post-insertion, the site showed stable, healthy soft tissue and shallow probing depths.

SINGLE TOOTH RESTORATION WITH AN INDIVIDUALIZED SYMBIONIC TOOTH
A failing restoration (45–47) was removed, and a symbionic tooth was placed at site 46. All sites received single crowns. Six years post-op, site 46 showed healthy soft tissue.

IMMEDIATE PLACEMENT OF SYMBIONIC TEETH IN THE ESTHETIC ZONE
Failing restorations of teeth 11 and 21 were removed and the tooth roots extracted. Two symbionic teeth were immediately placed and later restored with single crowns.
SINGLE TOOTH RESTORATION IN A PATIENT WITH RISK FACTORS
Clinical situation
Tooth gap in region #35 following extraction elsewhere due to deep caries and acute pulpitis. The patient presented to the author’s practice eight weeks later requesting a fixed restoration. Slight horizontal ridge collapse. Soft-tissue thickness: 3 mm. Caries on adjacent crowned tooth #36.
Planned: symbionic tooth in region #35, treatment of tooth #36, and new single-tooth crowns on #35 and #36. Medical history included controlled Type 2 diabetes, smoking (20 cigarettes/ day), regular benzodiazepine use, and poor oral hygiene (BOP index: 38%).
Surgical solution
Modified mini-roll flap mobilized. Osteotomy prepared per protocol for D3 bone. Symbionic tooth inserted in region #35 at low speed with final torque of 11 Ncm.
Restorative solution
Glass fiber post cemented and prepared 3 months post-op. Full-arch impression taken. Partially veneered, individually characterized zirconia crowns cemented on symbionic tooth #35 and natural tooth #36.
Outcome
The follow-up after 4.5 years revealed a situation comparable to that of a healthy natural tooth, marked by healthy and stable soft tissue and shallow probing depths (Fig. 8).
Clinical situation
Tooth gap in region #35 following extraction elsewhere due to deep caries and acute pulpitis. The patient presented to the author’s practice eight weeks later requesting a fixed restoration. Slight horizontal ridge collapse. Soft-tissue thickness: 3 mm. Caries on adjacent crowned tooth #36.
Planned: symbionic tooth in region #35, treatment of tooth #36, and new single-tooth crowns on #35 and #36. Medical history included controlled Type 2 diabetes, smoking (20 cigarettes/ day), regular benzodiazepine use, and poor oral hygiene (BOP index: 38%).
Surgical solution
Modified mini-roll flap mobilized. Osteotomy prepared per protocol for D3 bone. Symbionic tooth inserted in region #35 at low speed with final torque of 11 Ncm.
Restorative solution
Glass fiber post cemented and prepared 3 months post-op. Full-arch impression taken. Partially veneered, individually characterized zirconia crowns cemented on symbionic tooth #35 and natural tooth #36.
Outcome
The follow-up after 4.5 years revealed a situation comparable to that of a healthy natural tooth, marked by healthy and stable soft tissue and shallow probing depths (Fig. 8).
SINGLE TOOTH RESTORATION WITH AN INDIVIDUALIZED SYMBIONIC TOOTH
Clinical situation
Tooth gap in region #35 following extraction elsewhere due to deep caries and acute pulpitis. The patient presented to the author’s practice eight weeks later requesting a fixed restoration. Slight horizontal ridge collapse. Soft-tissue thickness: 3 mm. Caries on adjacent crowned tooth #36.
Planned: symbionic tooth in region #35, treatment of tooth #36, and new single-tooth crowns on #35 and #36. Medical history included controlled Type 2 diabetes, smoking (20 cigarettes/ day), regular benzodiazepine use, and poor oral hygiene (BOP index: 38%).
Surgical solution
Modified mini-roll flap mobilized. Osteotomy prepared per protocol for D3 bone. Symbionic tooth inserted in region #35 at low speed with final torque of 11 Ncm.
Restorative solution
Glass fiber post cemented and prepared 3 months post-op. Full-arch impression taken. Partially veneered, individually characterized zirconia crowns cemented on symbionic tooth #35 and natural tooth #36.
Outcome
The follow-up after 4.5 years revealed a situation comparable to that of a healthy natural tooth, marked by healthy and stable soft tissue and shallow probing depths (Fig. 8).
Clinical situation
Tooth gap in region #35 following extraction elsewhere due to deep caries and acute pulpitis. The patient presented to the author’s practice eight weeks later requesting a fixed restoration. Slight horizontal ridge collapse. Soft-tissue thickness: 3 mm. Caries on adjacent crowned tooth #36.
Planned: symbionic tooth in region #35, treatment of tooth #36, and new single-tooth crowns on #35 and #36. Medical history included controlled Type 2 diabetes, smoking (20 cigarettes/ day), regular benzodiazepine use, and poor oral hygiene (BOP index: 38%).
Surgical solution
Modified mini-roll flap mobilized. Osteotomy prepared per protocol for D3 bone. Symbionic tooth inserted in region #35 at low speed with final torque of 11 Ncm.
Restorative solution
Glass fiber post cemented and prepared 3 months post-op. Full-arch impression taken. Partially veneered, individually characterized zirconia crowns cemented on symbionic tooth #35 and natural tooth #36.
Outcome
The follow-up after 4.5 years revealed a situation comparable to that of a healthy natural tooth, marked by healthy and stable soft tissue and shallow probing depths (Fig. 8).
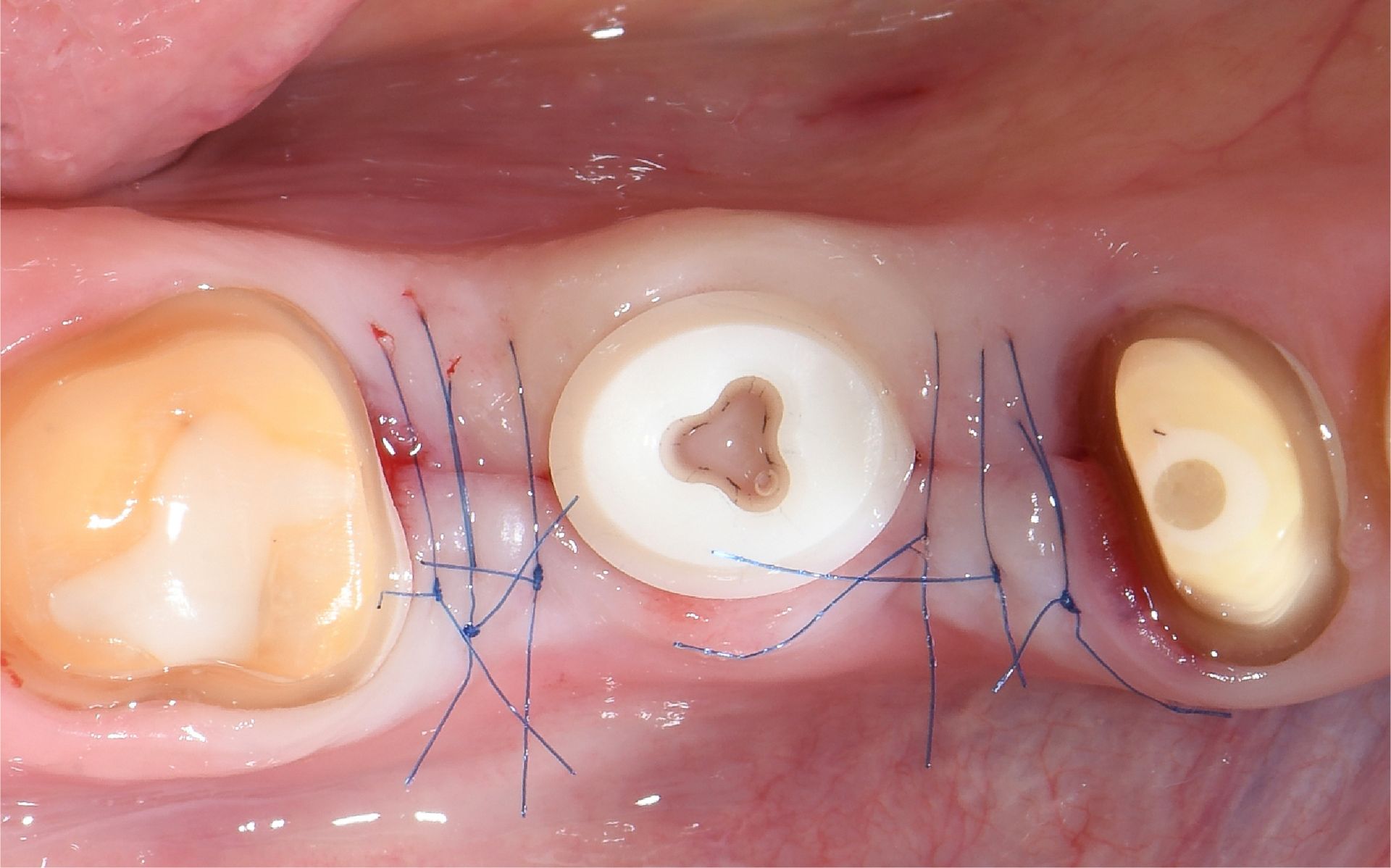
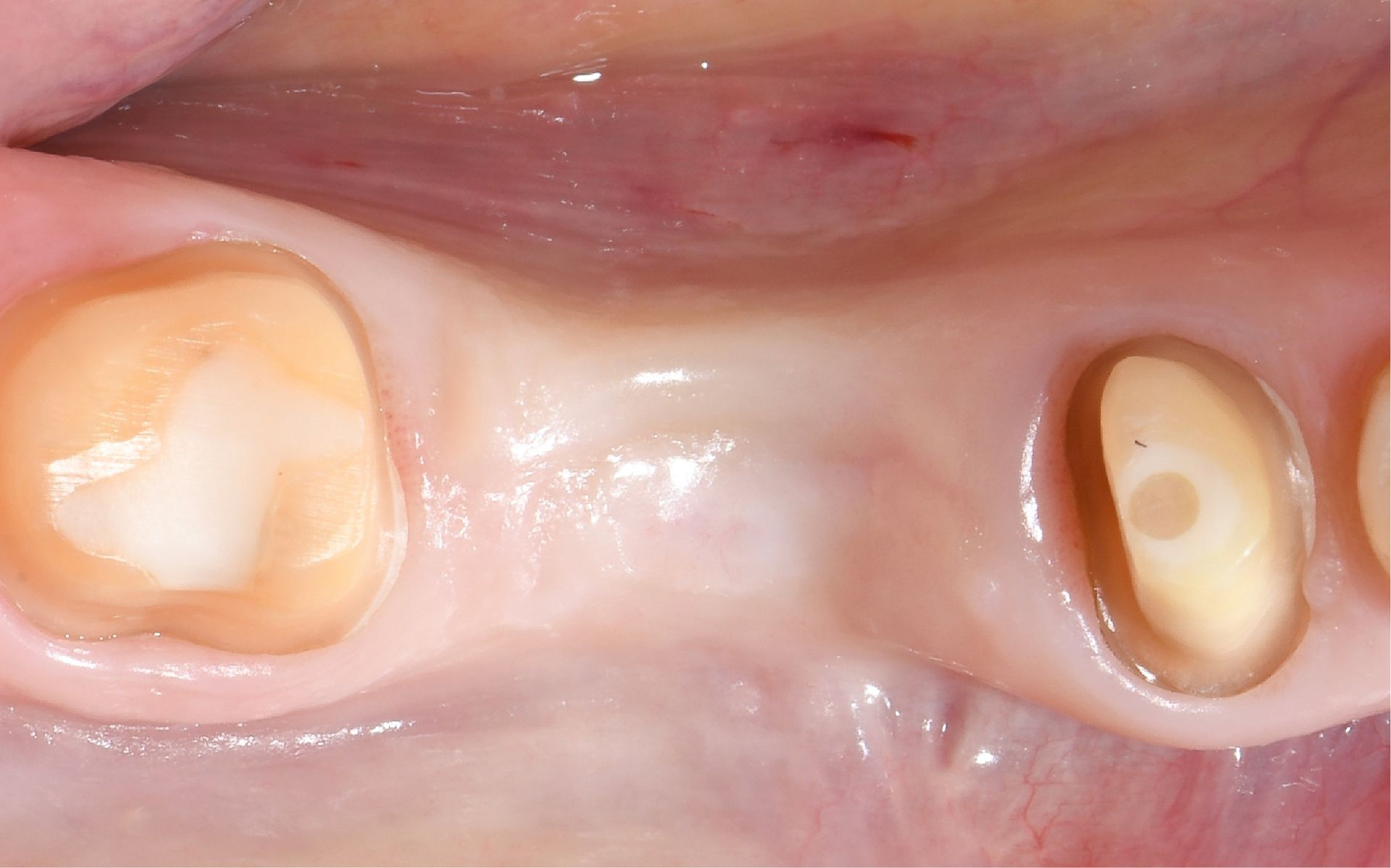
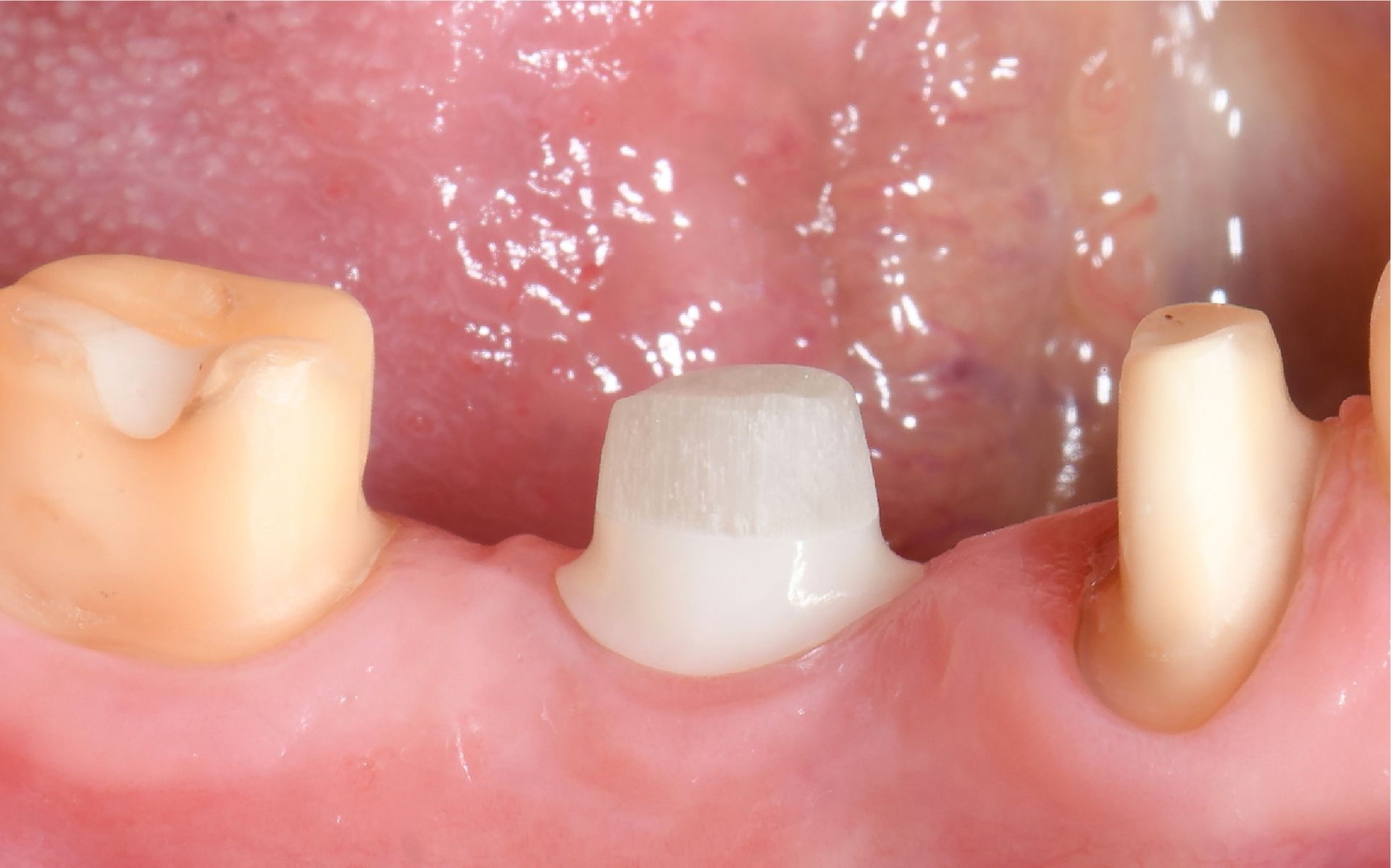
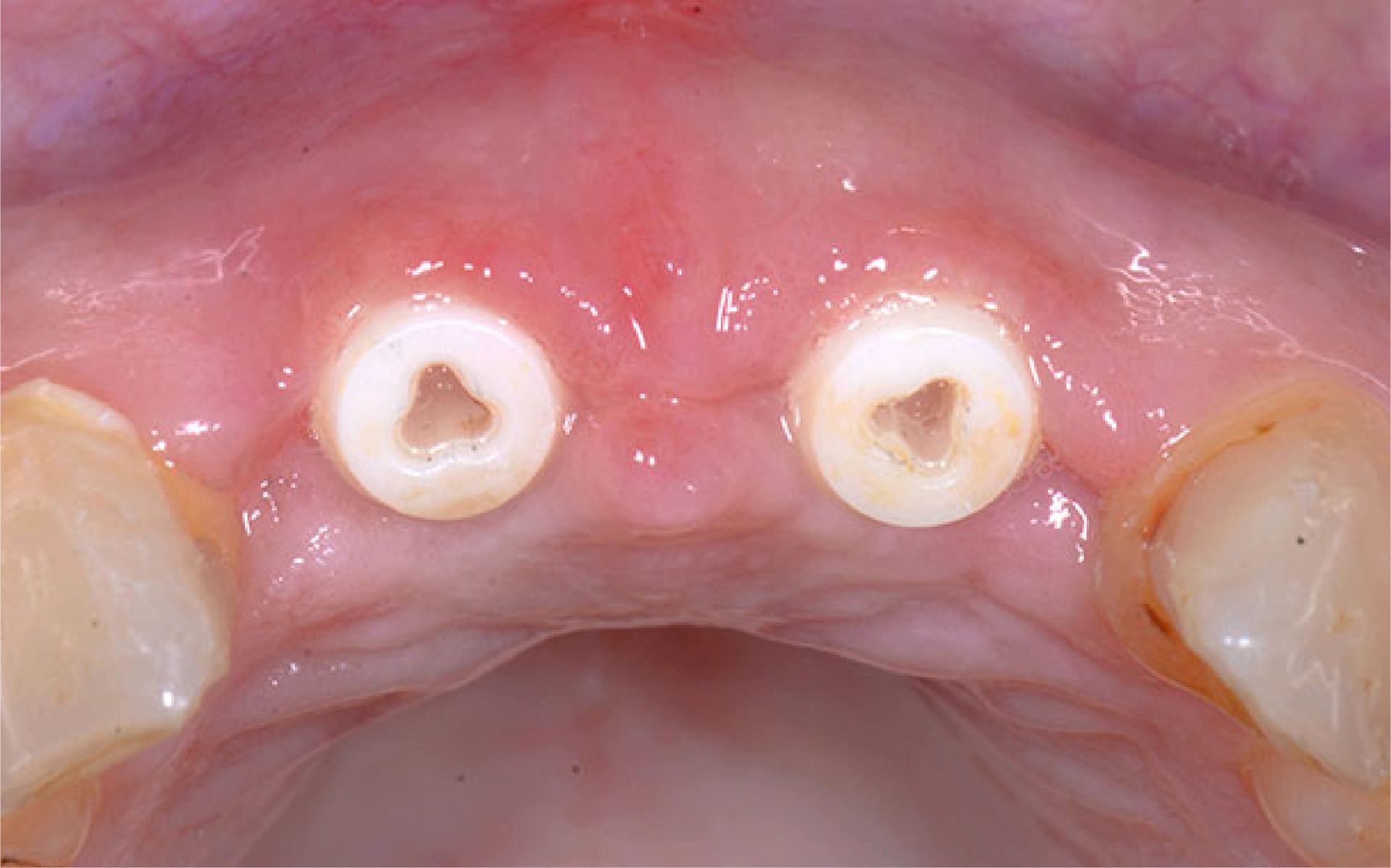
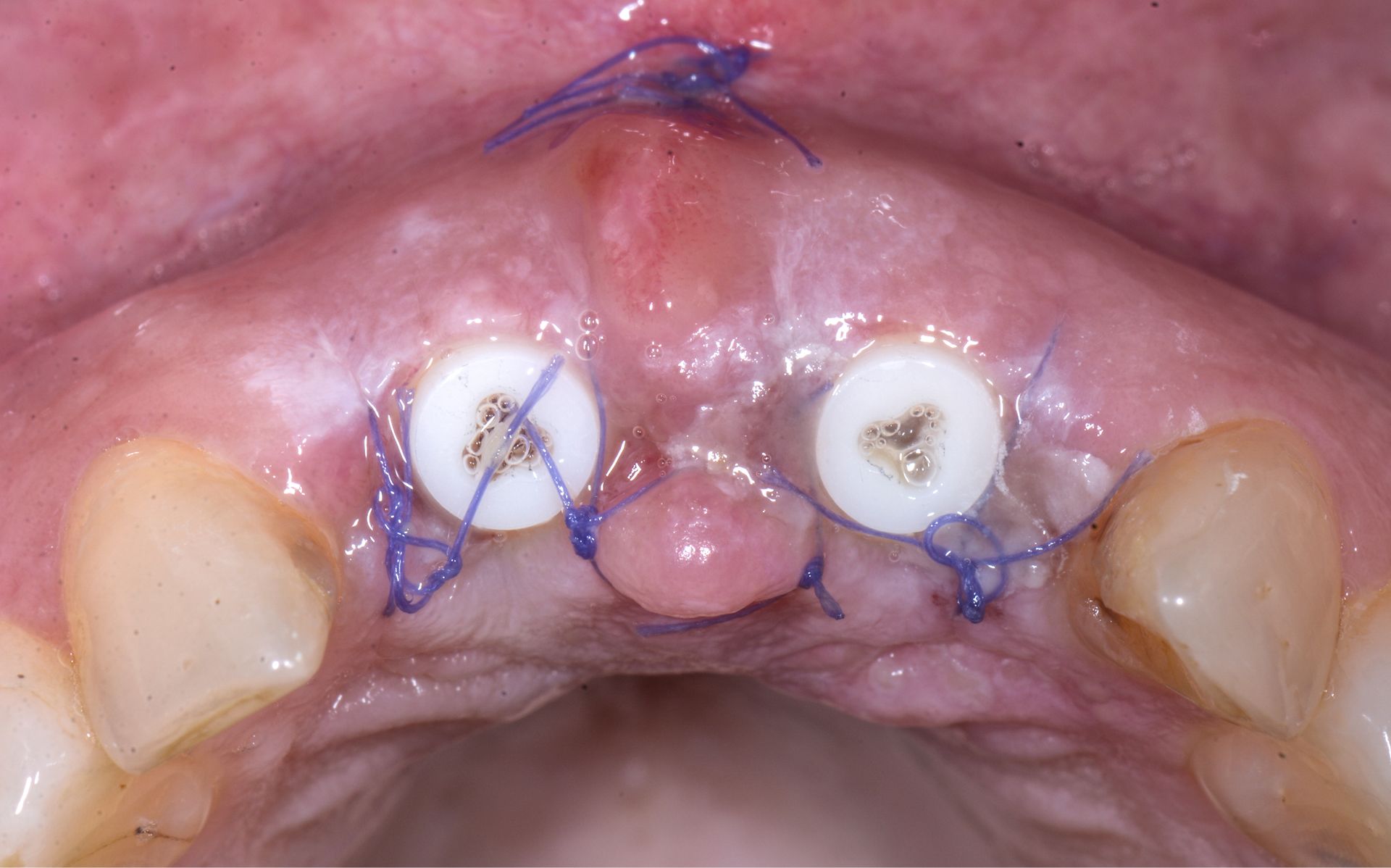
IMMEDIATE PLACEMENT OF SYMBIONIC TEETH IN THE ESTHETIC ZONE
IMMEDIATE PLACEMENT OF SYMBIONIC TEETH IN THE ESTHETIC ZONE
Clinical situation
Failing post-and-core restorations of teeth #11 and #21 required replacement. The patient requested a fixed tooth replacement solution. Planned treatment included removal of the failing restorations, extraction of the remaining tooth roots, immediate placement of two Patent™ Symbionic Teeth, and restoration with final crowns following successful integration.
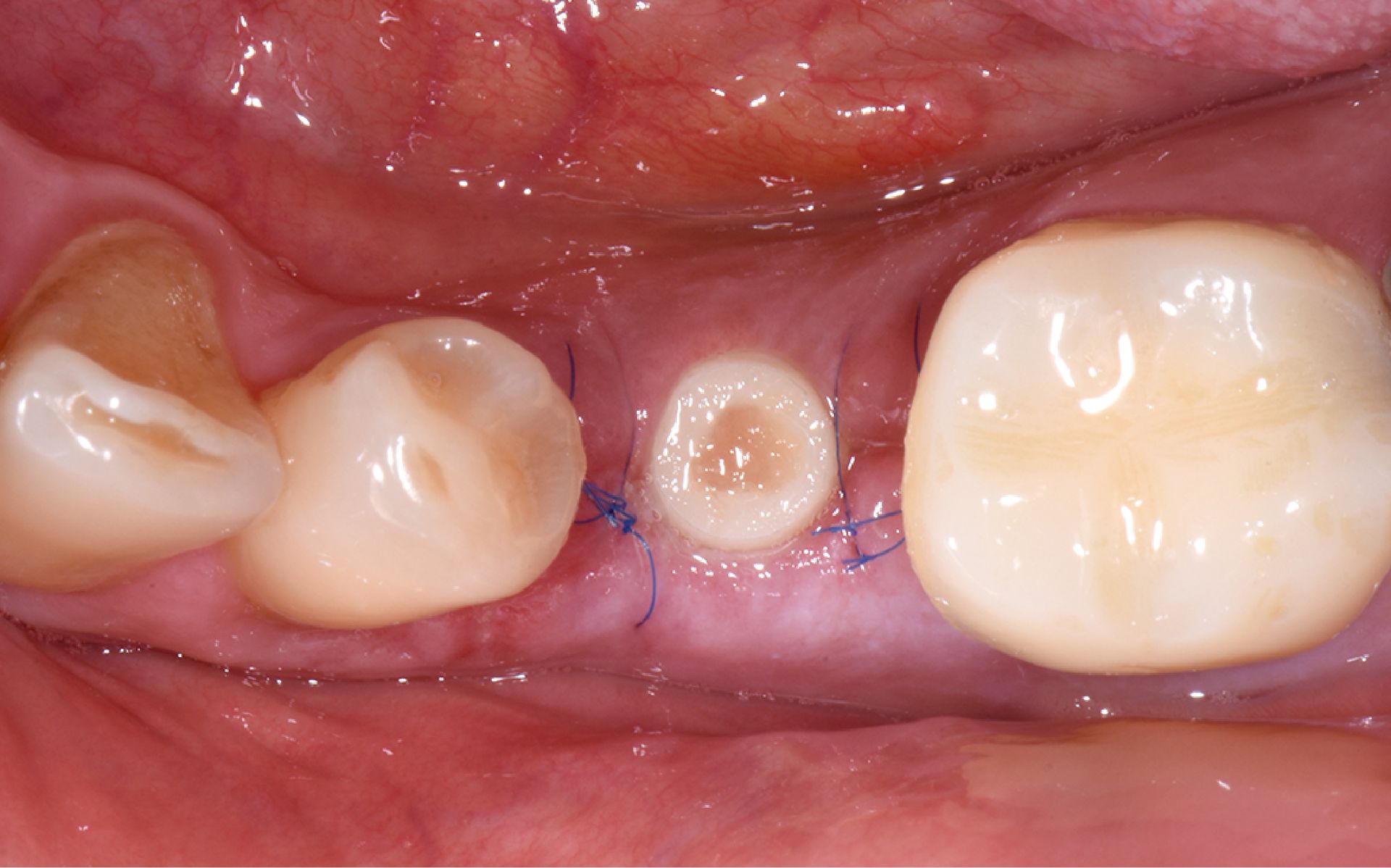
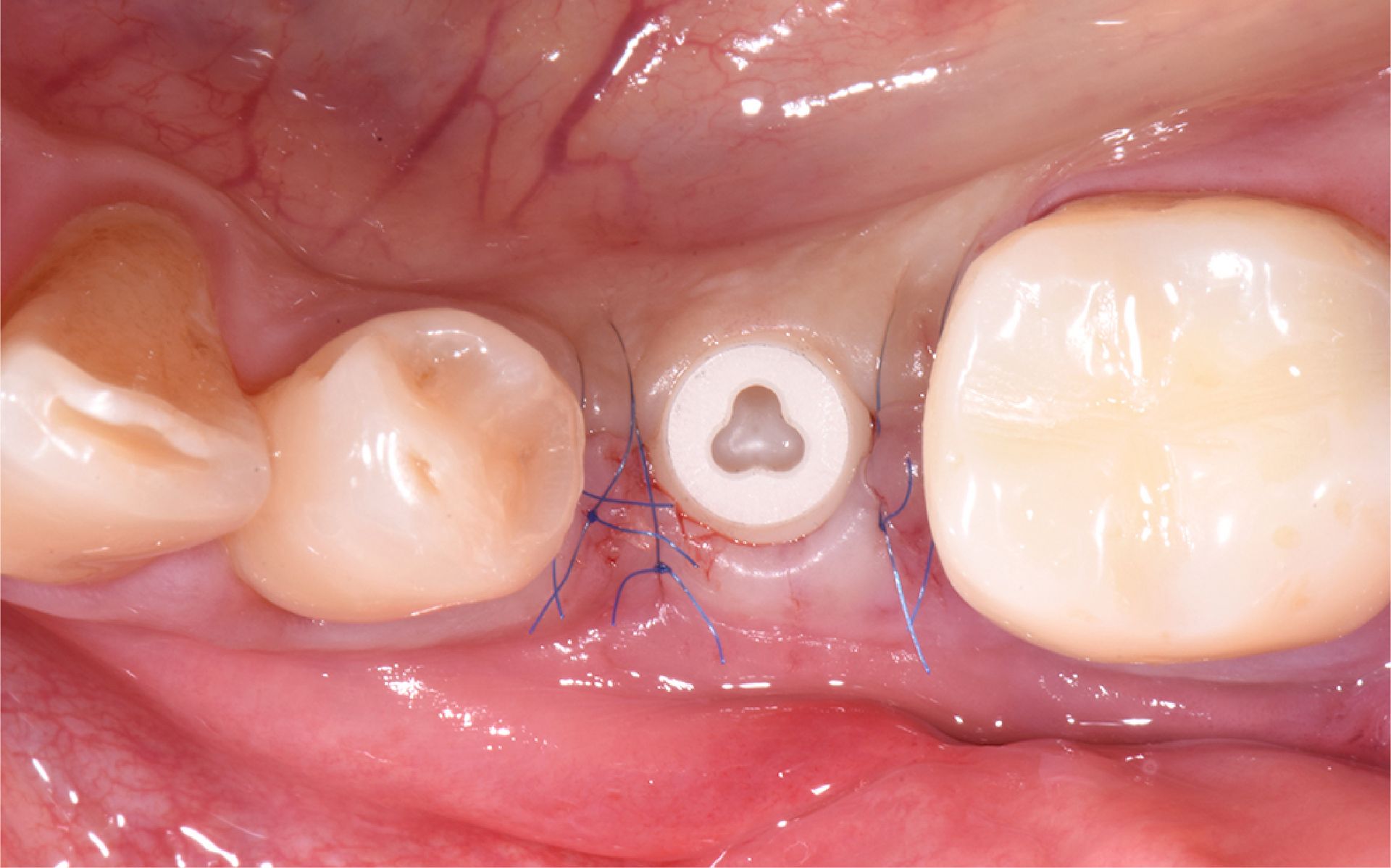
Surgical solution
Vestibular incisions were made in regions #11 and #21. The old restorations were removed, and the tooth roots were extracted. The alveoli were curetted. A surgical guide was placed, and osteotomies were prepared according to the manufacturer’s protocol for D3 bone at 600 RPM. Symbionic Teeth were
inserted to moderate final torque.
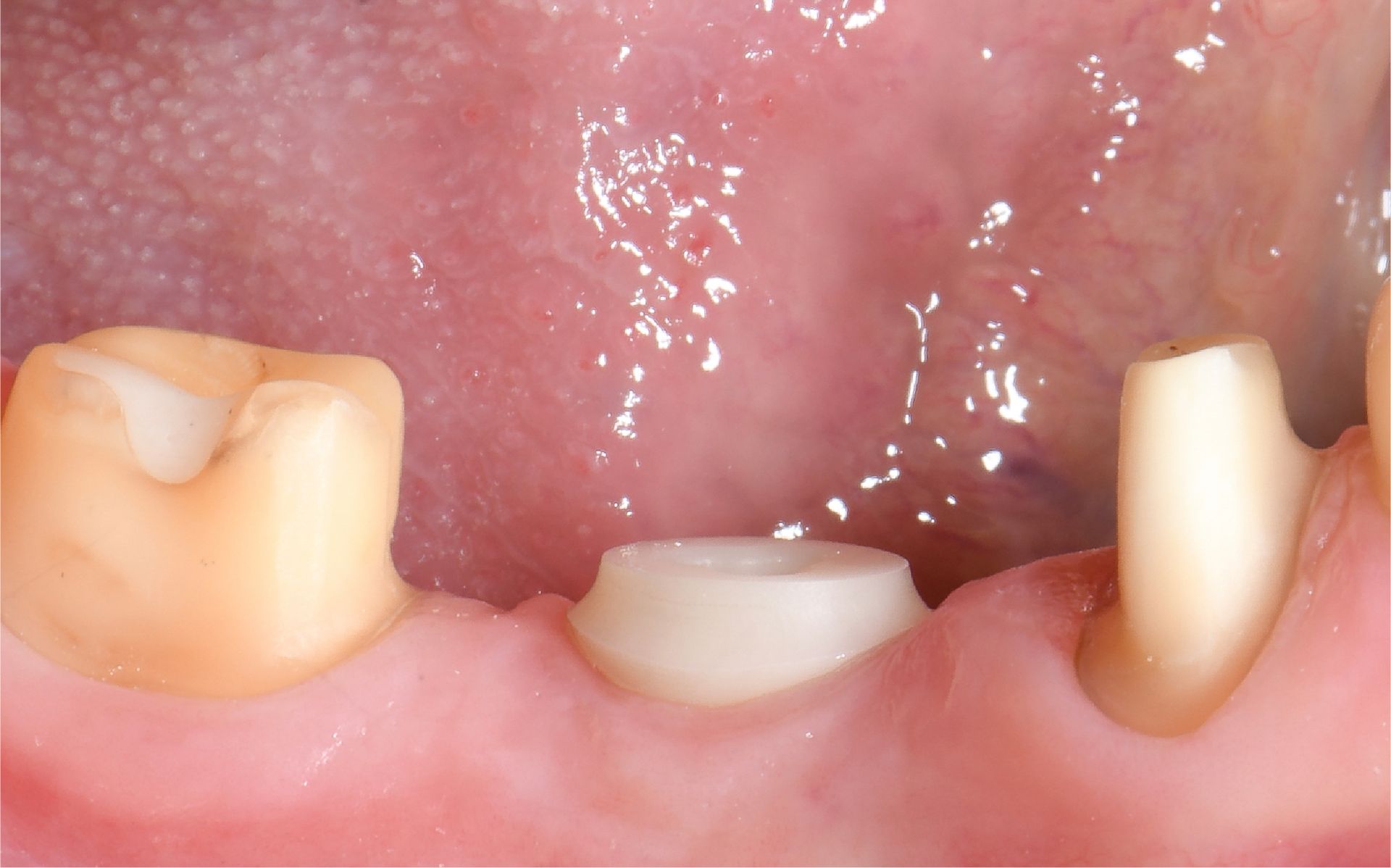
Restorative solution
Glass fiber posts were cemented and prepared 2 months post-surgery. A digital impression of the entire arch, including the prepared posts, was taken using an intraoral scanner. The posts were isolated with glycerin oil, and provisional crowns were cemented using a temporary cement mixture.
Final crowns were delivered after 3 months of healing.
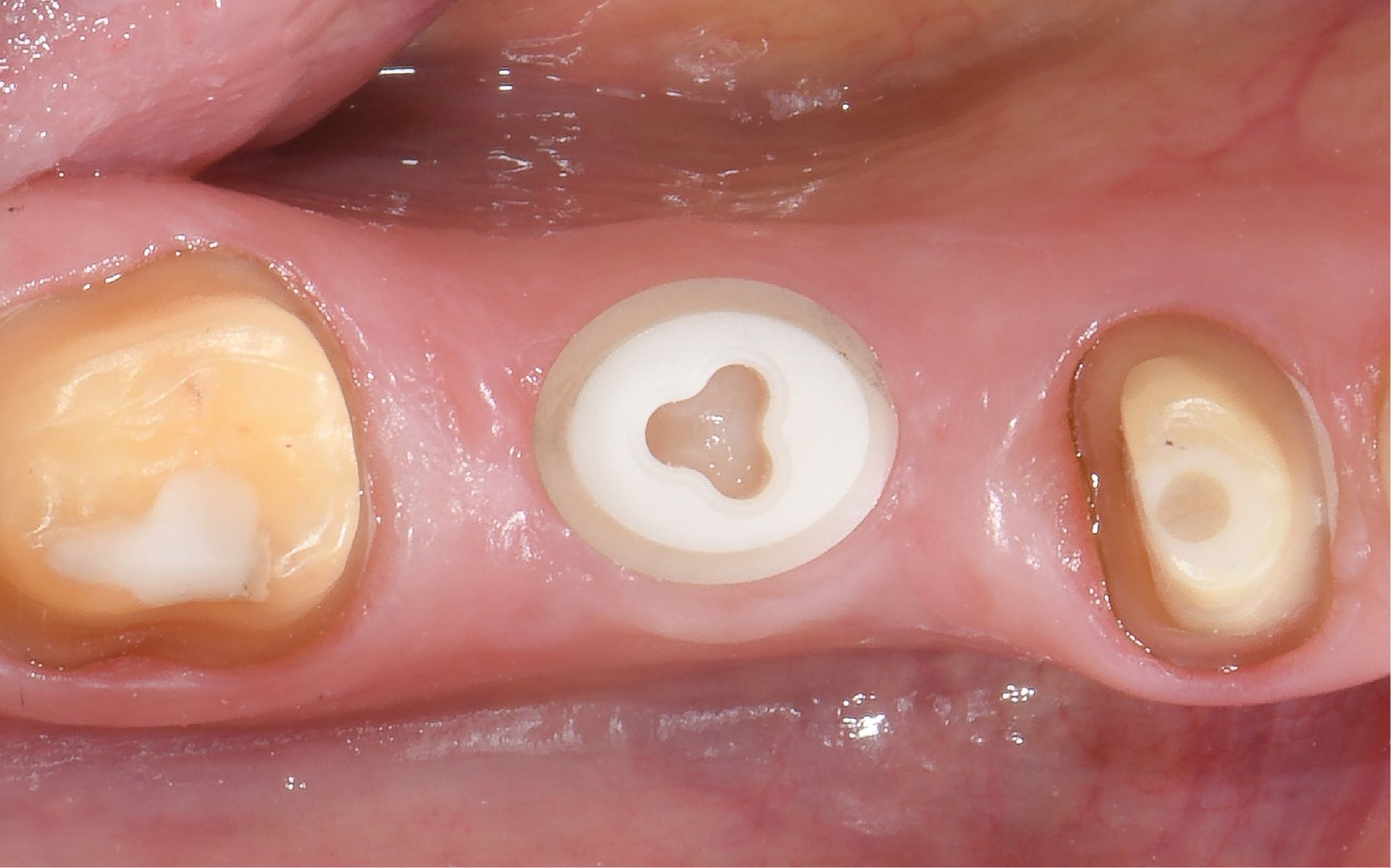
Outcome
At the 3-year follow-up (Fig. 10), the situation is characterized by healthy and stable soft tissue, resulting in excellent esthetics.
Clinical situation
Failing post-and-core restorations of teeth #11 and #21 required replacement. The patient requested a fixed tooth replacement solution. Planned treatment included removal of the failing restorations, extraction of the remaining tooth roots, immediate placement of two Patent™ Symbionic Teeth, and restoration with final crowns following successful integration.
Surgical solution
Vestibular incisions were made in regions #11 and #21. The old restorations were removed, and the tooth roots were extracted. The alveoli were curetted. A surgical guide was placed, and osteotomies were prepared according to the manufacturer’s protocol for D3 bone at 600 RPM. Symbionic Teeth were
inserted to moderate final torque.
Restorative solution
Glass fiber posts were cemented and prepared 2 months post-surgery. A digital impression of the entire arch, including the prepared posts, was taken using an intraoral scanner. The posts were isolated with glycerin oil, and provisional crowns were cemented using a temporary cement mixture.
Final crowns were delivered after 3 months of healing.
Outcome
At the 3-year follow-up (Fig. 10), the situation is characterized by healthy and stable soft tissue, resulting in excellent esthetics.