
Dr. Fabio Rossi
Via Amendola Giovanni 12
Bologna
40121
Italy
Studio Dentistico
Dr. Filippo Battelli
Via Manzoni 2
S. Andrea in Casale
Rimini
47832
Italy
Studio Dentistico

Initial situation
The 55-year-old female patient presented to practice in November 2021. Owing to failing post and core restorations of endodontically treated teeth #11 and 21, she expressed the desire for an implant-supported restoration in this area. The radiographic evaluation by means of CBCT revealed that there was sufficient bone volume in sites #11 and 21 for the planned implant placement (Fig. 1).
Treatment planning
Digital planning of the implant positioning and the design of the surgical guide were conducted using coDiagnostiX planning software (Dental Wings; Fig. 2). As part of the surgical procedure, it was planned to remove the failing restorations, extract the remaining tooth roots, and insert two-piece zirconia implants (Patent™ Dental Implant System, Zircon Medical Management) immediately into the extraction sockets. The implants were planned to be left for transmucosal healing. It was further planned to restore implants #11 and 21 with a provisional restoration supported by the neighboring teeth in order to protect the implants during healing and to provide esthetics. This would allow the patient to leave the practice after implant surgery without obviously missing crowns. Also, it was planned to cement and prepare the glass fiber post and core assemblies, which serve as abutments of the two-piece implants used, once the implants had successfully integrated and healing had been completed.

Fig. 1: Initial radiograph.
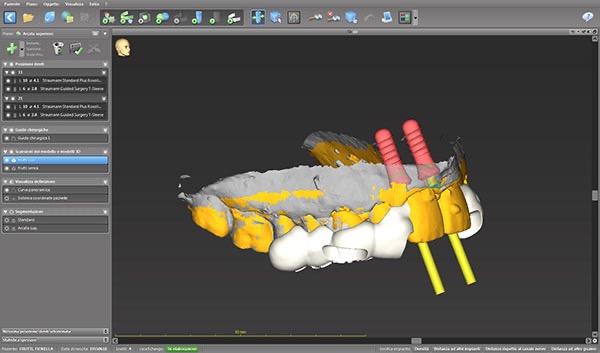
Fig. 2: Digital implant planning.
Surgical procedure
After local anesthesia had been administered to the patient, vestibular incisions were made in sites #11 and 21 to facilitate the removal of the old restorations (Fig. 3). After the old restorations had been removed, the underlying roots were extracted (Fig. 4). Thereafter, the extraction sockets were carefully curetted to completely remove any fibrous tissue. The surgical guide was then placed (Fig. 5), and the osteotomies were prepared according to the drilling protocol of the implant manufacturer and under water cooling (Fig. 6). Final drilling was done without the surgical guide in place. Once the osteotomies had been prepared, the implants, with a diameter of 4.1 mm and a length of 11.0 mm, were inserted into the osteotomies and screwed in using the insertion tool provided by the implant manufacturer, to a maximum torque of 35 N cm. Positioned at the equigingival level, the implants achieved sufficient primary stability (Figs. 7 & 8). The sites were carefully sutured (Fig. 9) before the provisional restoration was placed to protect the implants from occlusal stresses during healing and to provide esthetics (Fig. 10).

Fig. 3: Vestibular incisions.
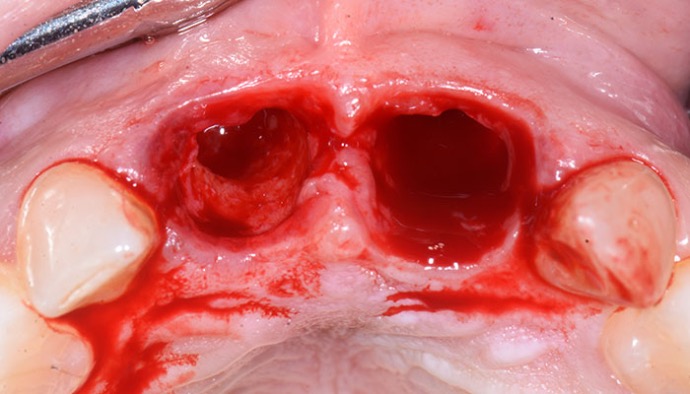
Fig. 4: Situation after root extraction.
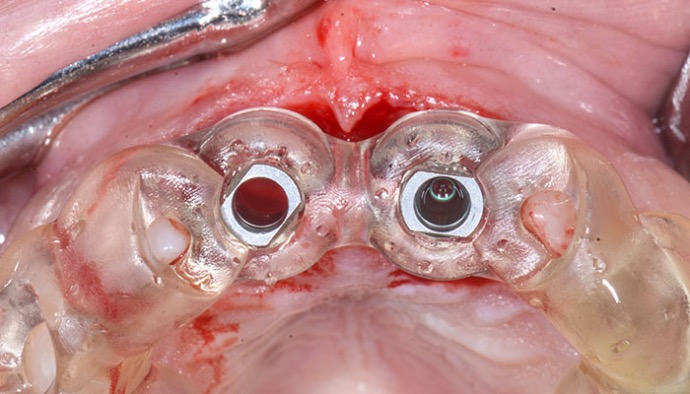
Fig. 5: Surgical guide in place.
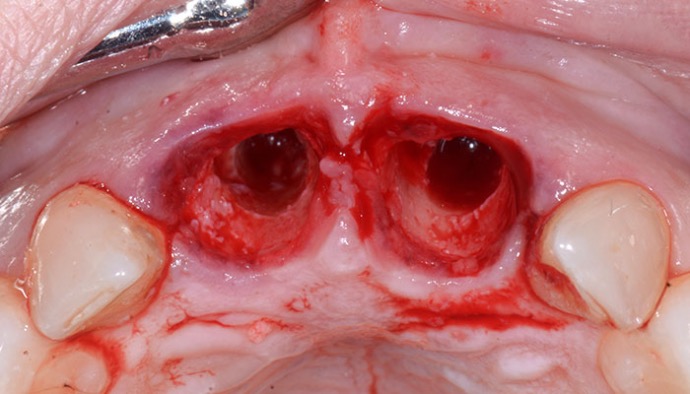
Fig. 6: Prepared osteotomies.

Fig. 7: Inserted implants.

Fig. 8: Post-op radiograph.

Fig. 9: Sutured sites.

Fig. 10: Frontal view of provisional restoration.
Healing and prosthetic restoration
At the three-day follow-up, healing was found to be uneventful. At the one-week follow-up, a favorable soft-tissue reaction around the placed implants was already visible (Fig. 11). After 30 days, healing was still uneventful (Fig. 12). After a successful healing period of two months, the 3C connections of the implants were cleaned, and dual-polymerizing cement (RelyX Universal, 3M ESPE) was applied to the prefabricated glass fiber posts before they were fitted into them (only a small amount of cement was applied to the posts to ensure that they go down properly). The cement was then light-polymerized. Subsequently, the cemented glass fiber posts were prepared to form intraorally using a high-speed diamond bur (Fig. 13). Excess cement was thoroughly removed. A digital impression of the entire arch, including the prepared glass fiber posts, was taken using an intraoral scanner, which served as the basis for the fabrication of the definitive crowns by the dental laboratory (Fig. 14). Thereafter, the prepared posts were isolated with glycerin oil, and new provisional crowns were subsequently cemented on to them using a temporary cement mixture (Fig. 15). After three months of healing, the definitive crowns were delivered (Fig. 16). At the follow-ups one week and one month after the delivery of the definitive prostheses, creeping attachment of the soft tissue and a visible increase in gingival volume were observed (Figs. 17 & 18). At the six-month follow-up, the soft-tissue conditions were considered healthy and stable, and the treatment result was deemed highly satisfactory from an esthetic point of view (Fig. 19).
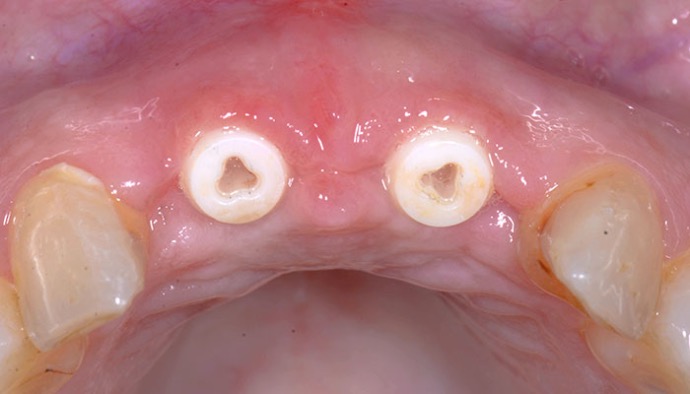
Fig. 11: Situation after one week.
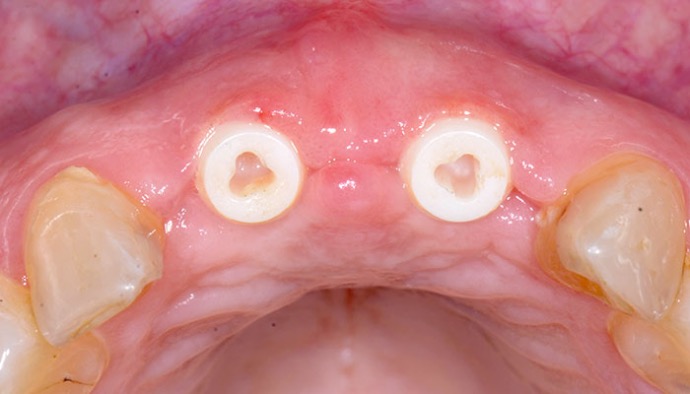
Fig. 12: Situation after one month.

Fig. 13: Prepared posts.
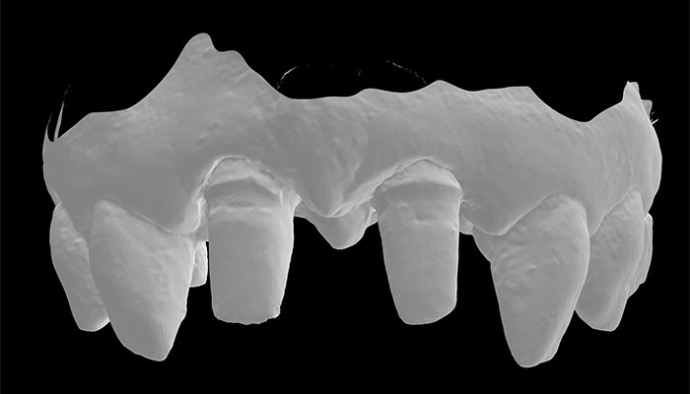
Fig. 14: Digital impression after two months.

Fig. 15: Delivery of new provisional crowns after two months.

Fig. 16a: Delivery of definitive crowns after three months: Clinical view.
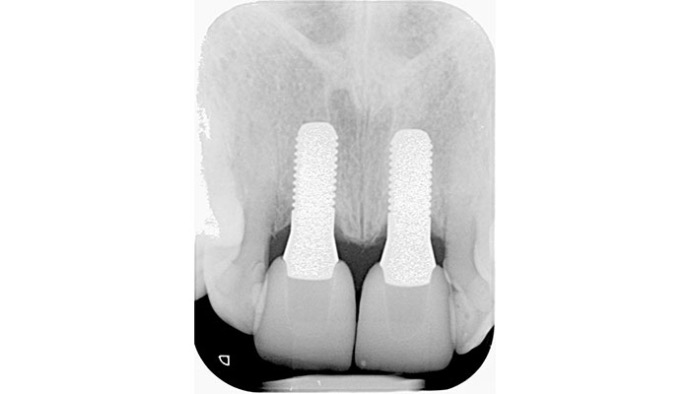
Fig. 16b: Delivery of definitive crowns after three months: Radiographic view.

Fig. 17: Situation one week after delivery of definitive crowns.

Fig. 18: Situation one month after delivery of definitive crowns.
Conclusion
With the two-piece zirconia implant system used in the clinical case described, highly esthetic restorations in the anterior area can be realized thanks to its natural-looking color and its beneficial soft-tissue integration. Also, thanks to its soft-tissue-level design, which avoids a microgap at the subgingival level, and the tissue-friendly and plaque-resistant implant material zirconia, long-term successful treatment outcomes with minimal risk for late biological complications such as peri-implantitis can be expected.

Fig. 19a: Situation three months after delivery of definitive crowns: Clinical view.

Fig. 19b: Situation three months after delivery of definitive crowns: radiographic view.





